The Lymphedema Treatment Act (LTA) is a federal law that went into effect on January 1, 2024. It requires Medicare to cover compression garments and supplies when prescribed for patients diagnosed with lymphedema.
Compression is the cornerstone of lymphedema treatment, but prior to the implementation of the LTA, Medicare was unable to cover these medical items. Here’s why:
Yes, all Medicare Advantage (MA) plans are required to cover anything that Original Medicare does, but the details of the coverage can vary significantly. Things such as allowable quantities, replacement frequencies, reimbursement rates, in-network suppliers, and other details are determined by each individual Medicare Advantage plan and can vary significantly from the coverage offered under Original Medicare. It’s important to research these differences when choosing your plan each year. Please see our Medicare Advantage page for further information.
No, the LTA has no jurisdiction over private or group health insurance plans, Medicaid, TriCare, or Veterans Affairs, however, most plans eventually follow the precedent set by Medicare. If your insurance plan is not yet providing the same comprehensive coverage you should contact them and urge them to align with the new Medicare precedent, as well as appeal any denial you receive citing current Medicare policy. You can report your denials here and LAG will use this information to help guide our advocacy efforts.
Medicare beneficiaries are able to get their compression garments and supplies from any Medicare DMEPOS supplier, whether a brick-and-mortar business or an online supplier. Those with other types of policies should contact their plans for a list of in-network suppliers.
To help you find a supplier that’s right for you, we have a Lymphedema Supplier Directory.
Suppliers have flexibility in both the products they offer and the insurance plans they accept. Some may only carry certain types of compression garments, while others may limit which insurers they work with—including Original Medicare and Medicare Advantage plans.
To help you find a supplier that’s right for you, we have a Lymphedema Supplier Directory.
No, suppliers cannot charge “upgrade” fees for compression garments covered under Medicare. More details on this topic are coming soon!
That depends on the supplier. Some accept measurements from therapists while others require that the measurements be taken by a member of their staff.
To help you find a supplier that’s right for you, we have a Lymphedema Supplier Directory.
Compression supplies are covered under Medicare Part B, and like all medical supplies covered under Part B the patient must first meet their deductible and is then responsible for 20% of the Medicare Fee Schedule amount for the respective product*.
If you have a secondary or supplemental Medicare Plan, it should help cover the patient responsible. Medicare Advantage plans coverage may vary. Private insurance plans differ, but likewise, whatever your out-of-pocket responsibility is for other covered medical supplies you should expect that it will be the same for your compression garment and supplies. The reimbursement rates are included in the 2025 DMEPOS Fee Schedule.
*To understand when a supplier would be allowed to charge more than the Medicare Fee Schedule amount please see the remaining questions in this section.
A Medicare “participating” supplier can only charge the Medicare approved amount for an item, because they are required to accept claims “on assignment.” A “non-participating” Medicare provider has the option to either accept a claim “on assignment” or charge a higher rate and pass that additional cost onto the patient. For further information please see Does Your Provider Accept the Medicare Rate as Full Payment?
When a Medicare supplier accepts a claim “on assignment” it means that they can only charge you the Medicare-approved amount, they will submit your claim directly to Medicare, they also cannot ask you to pay in full up front, and you are only responsible for your 20% plus any unmet deductible. For further information please see Does Your Provider Accept the Medicare Rate as Full Payment?
Yes, to qualify for coverage of compression supplies a Medicare beneficiary will have to have a diagnosis of lymphedema. CMS lists the following diagnosis codes in the final rule.
You will need a prescription (in addition to a lymphedema diagnosis) in order to be eligible for coverage. Any authorized practitioner can prescribe the item(s).
How often you need a new prescription depends on the insurance plan. A new prescription may be required annually by private payers, Medicaid, etc.
For Medicare, a new prescription is not required if the details have not changed (exceptions and details further defined in the article link), but timely documentation (i.e., a medical record note once every 12 months) is required. Documentation is not limited to a lymphedema therapist; it can be from other clinicians as well.
In order to be eligible for coverage you must have a lymphedema diagnosis and a prescription for your compression supplies, but these do not need to come from a specialist. Your primary care physician or other qualified healthcare provider can provide these things. Our Provider Handout may be helpful if your doctor needs further information.
If your doctor is unfamiliar with the Lymphedema Treatment Act or unsure how to prescribe covered compression item share our Provider Handout – it clearly explains diagnosis, prescription, and documentation requirements for Medicare coverage. Clear documentation and a correct prescription are essential for coverage—your provider plays a key role, and we’re here to help them succeed.
To obtain coverage, clinical documentation must justify the medical necessity of the prescribed compression items, especially for custom-fit garments. Documentation can come from various healthcare providers, including physicians, hospitals, nursing facilities, home health agencies, or other healthcare professionals. It’s essential that the records clearly support the need for the specific items prescribed.
Medicare covers custom fitted (custom or non-standard) gradient compression garments. Custom fitted gradient compression garments are uniquely sized and shaped to fit the exact dimensions of the affected extremity of an individual to provide accurate gradient compression to treat lymphedema. Examples of scenarios where a custom fitted gradient compression garment might be used (not all-inclusive) are:
There must be documentation in the beneficiary’s medical record necessitating the use of a custom fitted gradient compression garment versus an off-the-shelf standard gradient compression garment.
Seeing a lymphedema therapist is not a requirement for Medicare coverage, but you do need to have a lymphedema diagnosis and prescription for the item(s).
No, Lipedema or Venous Insufficiency diagnosis alone does not qualify a patient for eligibility. However, anyone with a lymphedema diagnosis, regardless of cause, will be eligible for coverage. So, lipedema patients who also have a lymphedema diagnosis are eligible.
Original Medicare will cover the following:
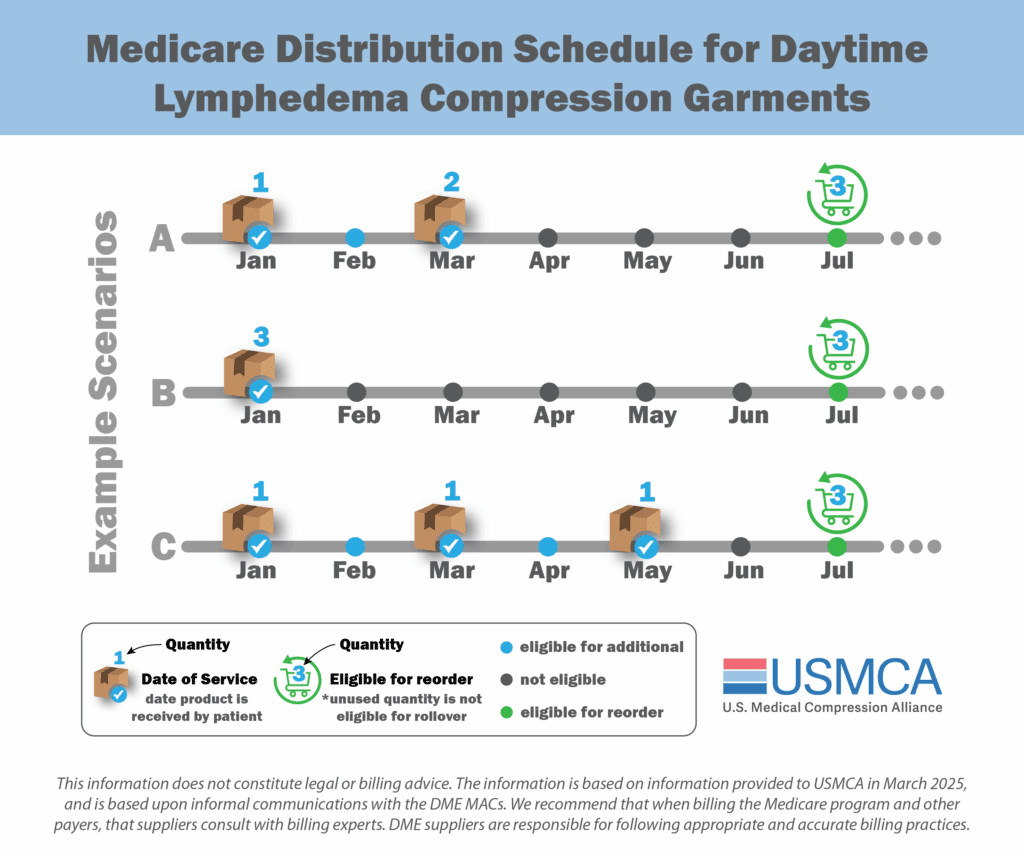
Medicare will cover compression sooner to replace lost, stolen, or irreparably damaged items or if a patient’s condition changes, like a change in limb size. As it is with coverage for any item or service under any insurance policy, there is always an appeals process whereby patients can seek exceptions.
If you use a Medicare supplier who accepts the claim “on assignment” then by law they cannot make you pay in full up front. If you use a Medicare “non-participating” supplier who does not accept the claim “on assignment” then they might make you pay the full amount up front. For further information please see Does Your Provider Accept the Medicare Rate as Full Payment?
No, patients are not required to get the maximum number of sets and can choose to order less based on their medical needs and financial situation.
If your insurance denies coverage for prescribed compression garments or supplies, you have the right to appeal—and it’s important to do so. Here’s how to start:
Tip: If you’re on Medicare and your claim was denied, visit the official Medicare Claims, Appeals, and Complaints page to get started.
You can also report your denials here, which helps us track trends and advocate for better coverage.
No, however, Medicare beneficiaries should be aware that the Medicare therapy cap was lifted through passage of the Bipartisan Budget Act of 2018. More information on that is available here.
All other aspects of lymphedema treatment (whether covered or not) fall under other existing benefit categories and therefore could not be included in the LTA. Therefore, the LTA does not change the status of coverage for any other supply, device, or medical service or procedure.
Yes, all lymphedema compression items have corresponding billing codes. Most items have specific codes based on the garment type and body part. For less common items, “not otherwise specified” (NOS) codes are used. These NOS codes do not have predetermined reimbursement amounts; instead, payment is determined on a claim-by-claim basis, considering the submitted invoice. New codes are added as necessary; for instance, six new codes became effective on April 1, 2025. For detailed information, refer to the complete DME fee schedule for lymphedema compression items.
Please see the PDAC Product Classification List (PCL) to determine which products are aligned under which code. It’s publicly available information and specifies which manufacturer products have been “code verified” by PDAC. Simply enter the HCPCS code of choice and it will show you all the manufacturer products that have been approved under that code.
Recognizing that most standard fit garments are circular knit, and most custom fit garments are flat knit, CMS decided that at this time the codes would be based solely upon whether an item was standard or custom fit, not the knit of the fabric. Their reasoning on this topic was outlined in the Final Rule. Codes for these distinct products may be added in the future.
Yes! The bill/law explicitly states, “standard and custom fitted gradient compression garments.”
Yes! Coverage for compression garments is per affected body area.
Yes. The final rule does not make any specifications to brands or manufacturers. Be certain to discuss your product preferences with the supplier when placing your order.
Yes. The new benefit category will cover the following:
No, the Lymphedema Treatment Act (LTA) does not change coverage for pneumatic compression pumps. These devices are considered durable medical equipment (DME) and are covered under a separate Medicare benefit category from compression garments and supplies.
Here’s what you need to know:
Note: The use of a pump is often considered when swelling is not sufficiently managed with garments alone, or in cases of severe lymphedema. However, coverage can vary by insurance plan, and preauthorization is often required.
For detailed guidance on pump coverage, including eligibility criteria and documentation requirements, visit the Medicare page for Lymphedema Pumps.
No, the Lymphedema Treatment Act (LTA) does not change coverage for compression supplies used in wound care unless the patient also has a diagnosis of lymphedema. Here’s the breakdown:
If you’re unsure whether your garment fits correctly:
Getting the right fit is critical to effective treatment—don’t hesitate to speak up if something feels off.
No, if you are on an insurance policy that is subject to the WHCRA then your plan must still conform to the requirements of the WHCRA. Learn more here.
Medicare’s 2025 rates are fixed for the year and will not change, even if tariffs are applied to lymphedema supplies. If you have Original Medicare and use a supplier that accepts assignment, you will not pay more than the Medicare-approved amount. However, suppliers who do not accept assignment may charge more, especially if their costs increase due to tariffs. Medicare adjusts its fee schedule annually based on factors like the Consumer Price Index for Urban Consumers (CPI-U). Other insurance plans set their own rates and may adjust them annually at their discretion.
Yes, there are footwear options for people with hard to fit feet (please see our Patient Resources page for this information) but no, these items are not covered by insurance. If you also have diabetes, however, you may qualify for coverage. Please see this post for more information.
Join our email list to learn about
changes to insurance coverage, advocacy actions,
new educational materials and more.
Subscribers receive approximately
one email per week with information
from both of our organizations.